From the Journal: Biomicrofluidics
WASHINGTON, June 9, 2020 — Human sweat contains several biomolecules the research community is exploring for noninvasive medical testing. Analyzing sweat for research, however, is often expensive, and devices typically are reliable for only a limited amount of time.
Researchers at North Carolina State University have constructed a paper-based device as a model of wearables that can collect, transport and analyze sweat in next-generation wearable technology. Using a process known as capillary action, akin to water transport in plants, the device uses evaporation to wick fluid that mimics the features of human sweat to a sensor for up to 10 days or longer. They discuss their work in the journal Biomicrofluidics, from AIP Publishing.
The work was a collaboration between Orlin Velev and Michael Dickey, advising the research of graduate students Timothy Shay and Tamoghna Saha, as part of the NSF Center for Advanced Self-Powered Systems of Integrated Sensors and Technologies. The goal is to use the properties of paper to point a way forward for more affordable, longer-term devices.
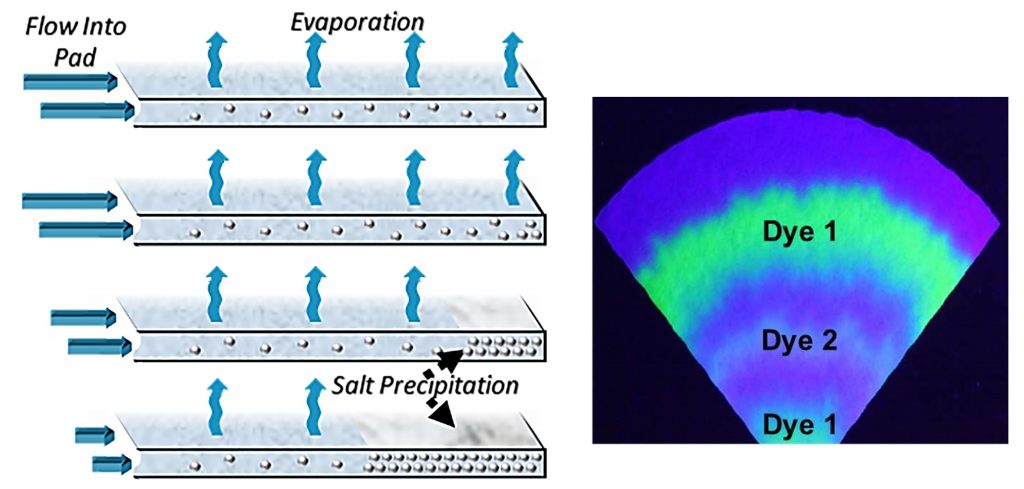
One central problem for any device in analyzing sweat is that sweat contains salt, which, upon evaporation, will become deposited on a device and interfere with fluid flow. The team’s device densely packs deposited salt crystals, allowing for longer use and a way to study the timing of when chemicals present in the sweat.
“We expected that the flow of the model sweat will be suppressed by the deposition of a salt layer inside the drying pad,” Velev said. “By following the flow of model sweat, we found, quite surprisingly, that such a simple paper construct can achieve continuous sweat pumping and disposal for very long periods.”
Paper microfluidic devices could also be used as wearable patches to assess the course of certain diseases or how well patients adhere to drug regimens.
“The biological markers or drug metabolites that seep in the patient’s sweat over a long period will be captured on the paper pad and preserved in a time-stamped manner to be analyzed later, similar to tree rings preserving the record of tree development,” Dickey said.
Driven by the liquid wicking through paper, the device doesn’t require external power. Its low cost also poses uses for inexpensive medical testing in under-resourced patient populations who struggle to have access to such testing. Such skin patch assays could remove the need to take blood samples.
The team has started a series of human trials to explore how the technology provides longer term biomarker analysis, and they look to resume the trials when pandemic safety measures make it feasible to proceed.
###
For more information:
Larry Frum
media@aip.org
301-209-3090
Article Title
Authors
Timothy Shay, Tamoghna Saha, Michael D. Dickey and Orlin D. Velev
Author Affiliations
North Carolina State University
