From the Journal: Applied Physics Reviews
WASHINGTON, May 4, 2021 — Spinal fusion is frequently performed to restore spinal stability in patients with spinal diseases, such as spinal stenosis, vertebral fractures, progressive deformities, and instability. In the past two decades, there has been marked increase in the number of people over 65 years in age who have needed spinal fusion surgery.
While autogenous bone grafts have long been considered the reference standard for spinal fusion, painful pseudoarthrosis remains a leading cause of poor clinical outcomes. Many researchers have consequently focused on trying to create a biomimetic scaffold that induces vascularization to enable bone tissue regeneration and spinal fusion.
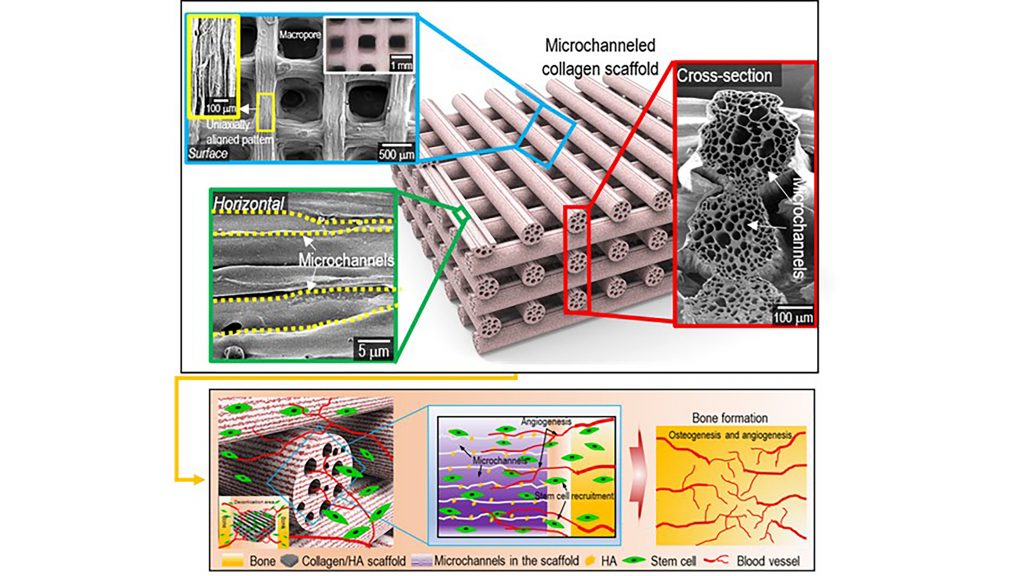
In Applied Physics Reviews, from AIP Publishing, researchers from Sungkyunkwan University in South Korea present a solution to address the challenge of fabrication of a biomimetic scaffold. The team designed a microchannel scaffold made of a collagen and hydroxyapitite combination, with each strut consisting of micrometer-scaled microchannels. The microchannels have induced growth of blood vessels in a mouse model.
“Since the fabrication of biomimetic scaffold is a challenging issue, the innovation of this study lies in adding extra hierarchy to the structure in the form of microchannels,” said author Geun Hyung Kim. “This was achieved through a 4D printing strategy, where one-way shape morphing is used.”
The researchers printed immiscible polymer blends that act as a double negative template in order to fabricate the the biomimetic collagen/hydroxyapatite hierarchical scaffold. They followed that by one-way shape morphing (4D printing) and coating processes.
Collagen is known as a hydrophilic material, and numerous in vivo studies have suggested it possesses excellent cellular activities. In the case of the microchanneled collagen/hydroxyapatite scaffold, the researchers noted significantly higher water-absorbing capability, compared to a conventional collagen scaffold, as a result of the capillary pressure supplied by the microchannels. Consequently, the in vivo studies have suggested excellent infiltration of cells into microchannels.
Going forward, the researchers will investigate enhancing the mechanical properties of the scaffold. Furthermore, controlling the mechanical properties of the scaffold would enable versatile applications of the microchanneled collagen/hydroxyapatite scaffold.
“I believe that the designed scaffold can have multiple applications with tubular structures such as muscle, tendon, and nerve,” said Kim.
Skeletal muscle is a hierarchical organization where the muscle fibers are encapsulated in microchannels known as endomysium. Therefore, the designed scaffold could act as endomysium to enable the infiltration of muscle fibers into the channels.
###
For more information:
Larry Frum
media@aip.org
301-209-3090
Article Title
Authors
Hanjun Hwangbo, Hyeongjin Lee, Eun Ji Roh, WonJin Kim, Hari Prasad Joshi, Su Yeon Kwon, Un Yong Choi, In-Bo Han, and Geun Hyung Kim
Author Affiliations
Sungkyunkwan University and CHA University School of Medicine
