Testing for glaucoma can create droplets that may carry viruses like SARS-CoV-2
From the Journal: Physics of Fluids
WASHINGTON, September 14, 2021 – A common eye test could expel tear droplets up to a meter away from the patient, potentially spreading viruses that cause COVID-19 and other pathogens.
In Physics of Fluids, by AIP Publishing, scientists from the Indian Institute of Science and the Narayana Nethralaya Foundation explain how tears ejected from the eye during a procedure that tests for glaucoma can theoretically transmit disease.
Ophthalmologists use a tonometer to measure the pressure in an eye. A high-pressure reading can indicate a risk for developing glaucoma. The instrument emits an air puff that hits the surface of the eye.
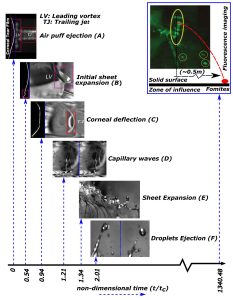
The researchers modeled the eye’s response to this puff and took high speed images of eyes undergoing the procedure. They were specifically looking at the liquid in the eye and how it responded.
As the eye was hit with the air puff, the film of tears on the surface expanded into a sheet that spilled out over the eyelids. The cornea also deflected away from the incoming air.
“The cornea is like an elastic surface. So, as it deforms and as it recovers its shape, it gives the eye an additional kick,” said author Saptarshi Basu. “It’s a capillary wave merged with this corneal deflection, which gives rise to a consolidated wave, and that is what makes the tear fluid expand and go out.”
The waves moving within the eye and tear liquid eventually become unstable, and the tears break up into droplets. The team tracked the speed of those droplets as they left the eye and predicted they could travel up to a meter away from the patient. The distance depends on the air flow within the room.
Eyes with more tears created more droplets than dry eyes. The scientists recommend not using eye drops before the glaucoma test unless medically necessary.
“It is not just limited to SARS-CoV-2. It can be extrapolated to other types of pathogens as well,” said Basu. “What you think is a very safe, noncontact procedure, even then, one needs to be a little careful.”
This work can help eye care practitioners to develop and follow health and safety protocols, like improved room ventilation and cleaning nearby instruments and surfaces, that may not have been considered necessary in the past.
###
For more information:
Larry Frum
media@aip.org
301-209-3090
Article Title
Authors
Saptarshi Basu, Durbar Roy, Sophia M, Abdur Rasheed, Prasenjit Kabi, Abhijit Sinha Roy, Rohit Shetty
Author Affiliations
Indian Institute of Science, Narayana Nethralaya Foundation
