New device may reduce the number of unnecessary biopsies by offering a fast, comprehensive and non-invasive examination of melanoma and other skin cancer lesions
From the Journal: Review of Scientific Instruments
WASHINGTON, D.C., August 5, 2014 – As thousands of vacationers hit the beach this summer, many of them will expose their unprotected bare limbs to direct UV sunlight, potentially putting them at risk of skin cancer later in life. To fight back, scientists can also turn to light, designing optical devices that may detect cancerous skin lesions early on, leading to better treatment outcomes and ultimately saving lives.
Researchers from the University of Texas at Austin’s Cockrell School of Engineering have now developed a probe that combines into one device three unique ways of using light to measure the properties of skin tissue and detect cancer. The researchers have begun testing their 3-in-1 device in pilot clinical trials and are partnering with funding agencies and start-up companies to help bring the device to dermatologists’ offices.
The researchers describe the skin cancer probe in a new paper published in the journal Review of Scientific Instruments, from AIP Publishing.
Skin cancers of all types are the most common forms of cancer in North America, and melanoma, the most deadly form of skin cancer, is one of the leading causes of cancer death, killing nearly 10,000 people every year in the United States.
Currently, the only definitive way to diagnose skin cancer is to perform a biopsy, in which doctors remove a suspect skin lesion and then examine the stained tissue under a microscope to look for cancerous cells. Determining which lesions to biopsy is an imprecise art, however, and for every case of skin cancer detected there are roughly 25 negative biopsies performed, translating to a cost of $6 billion to the U.S. health care system, according to estimations performed by the researchers.
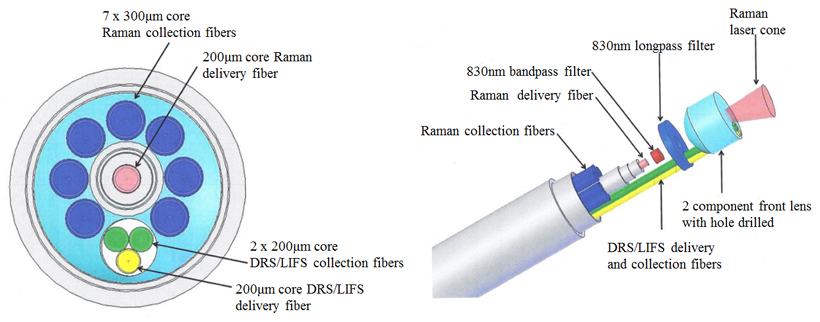
James Tunnell, an associate professor in the biomedical engineering department at UT, believes the new probe developed by his team could eventually help reduce the high number and cost of negative biopsies by giving a clear picture of which skin lesions are most likely cancerous. He and his colleagues combined three common spectroscopic techniques – Raman spectroscopy, diffuse reflectance spectroscopy, and laser-induced fluorescence spectroscopy – into one probe to create a more complete picture of a skin lesion. By revealing information invisible to the human eye, the probe could offer a better screening tool for cancer and eliminate many negative biopsies.
As normal skin becomes cancerous, cell nuclei enlarge, the top layers of skin can thicken and the skin cells can increase their consumption of oxygen and become disorganized, Tunnell said. The changes alter the way light interacts with the tissue.
To detect all these changes requires multiple spectroscopic techniques. For example, diffuse optical spectroscopy is sensitive to absorption by proteins such as hemoglobin while Raman spectroscopy is sensitive to vibrational modes of chemical bonds, such as those found in connective tissues, lipids, and cell nuclei, Tunnell noted.
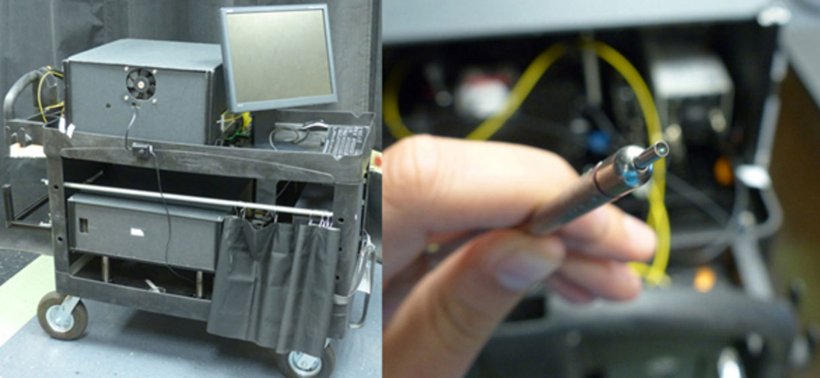
Previous research efforts have tried combining spectroscopic techniques to aid in skin cancer detection, but the University of Texas team is the first to combine three techniques in a single probe that would be inexpensive enough to be used widely in clinics and doctors’ offices. The probe itself is about the size of a pen and the spectroscopic and computer equipment that supports it fits neatly onto a portable utility cart that can be wheeled between rooms. Each reading takes about 4.5 seconds to perform. The 3-in-1 nature of the probe saves time and money while still giving a comprehensive examination of the skin properties.
“Skin is a natural organ to apply imaging and spectroscopy devices to because of its easy access,” Tunnell said. Most devices have been at the research stage for the last 10 years or so, but several are now undergoing clinical development, he noted. “This probe that is able to combine all three spectral modalities is the next critical step to translating spectroscopic technology to the clinic.”
###
For More Information:
Jason Socrates Bardi
American Institute of Physics
jbardi@aip.org
240-535-4954
@jasonbardi
Article Title
Authors
Manu Sharma, Eric Marple, Jason Reichenberg and James W. Tunnell
Author Affiliations
University of Texas at Austin, EmVision LLC, and the University of Texas Southwestern
